



As Sergeant Surgeon to King Charles II, Richard Wiseman (1622-1676) was present at many of the battles of the Civil War and he described the war wounds as follows: " Wounds made by gun-shot are the most complicate sort of wounds that can be inflicted: For they are not only solution of continuity, but have joined with them contusion. Attrition, and dilaceration, in a high and vehement kind. To this we may add all sorts of fractures and accidents, as haemorrhagia, inflammation, erysipelas, gangrene, and sphacelus; besides the extraneous bodies which are violently carried into the wound, and multiply indications". |
| During more that 50 years Colombia faced almost a civil war; I would not be able to exactly define in what kind of war we were living. Today (2017) this war is almost over. At the Military Hospital in Bogotá, we had to deal with war wounds caused mainly by: Fragmentation missiles (mortar, grenade shells), Solid missiles (low and high velocity bullets) and antipersonnel mines. With microsurgery we are able to transplant almost any kind of tissue to reconstruct difficult wounds; it is not an easy surgery but is the best way and some times the only way. The ironic issue is: this kind of lesions are created by the man, the etiology is the human being, so logically it would be easier to prevent them than prevent diseases like cancer. Probably men will find the way to prevent cancer but won't be able to stop the war. Hopefully the current peace process in Colombia will end the civil war (at least with the FARC). Because the Colombia Peace Process today is rare to see soldiers with war wounds. |
Muscular or musculocutaneous flaps were the choice for lower extremities and fasciocutaneous flaps the choice for upper extremities and face. Two osseocutaneous free flaps were used to restore the mandible in two patients.
Satisfactory results were obtained in 28 of the 32 cases.
Even though free flaps are essential to the reconstruction of severe war wounds, the severity of the damage to the surrounding tissues produced 12.5% failure rate in the 32 free flaps of the acute war-wounded group compared to 0% in the 54 free flaps of the non-war-wound group.
CONCLUSION:
In major and severe trauma, as the war wounds, the free flap reconstruction is a powerful tool. However, the cases must be carefully selected and the flap to use well indicated. The failure rate is higher than the free flaps used in non-war injuries, but is important to understand that these patients have limited or no other options of treatment, as shown in the clinical cases.
CLINICAL CASE 1.
HIGH VELOCITY GUNSHOT WOUND IN THE FOREARM

Preoperative picture: palmar view of the wound.

Preoperative picture: dorsal view of the wound.

Picture of the free flap, in fact there are to flaps (latissimus dorsi and scapular) with one pedicle (subscapular vessels). The radial artery and comitant veins are used as recipient vessels; the latissimus dorsi muscle is used to cover the palm and the scapular skin the dorsum.

Four month postoperative picture, palmar view. (Grafted Latissimus Dorsi muscle flap).

Four month postoperative picture, dorsal view. (Scapular skin flap).
CLINICAL CASE Nº 2.

Picture 1. Left leg amputation and open fracture of right leg. It is very important to save the right leg, in order to rehabilitate the patient.
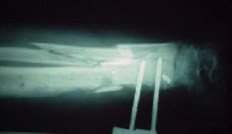
Picture 2. X Rays of the exposed tibia and fibula fracture.
ANTIPERSONNEL MINE IN THE LEGS


Picture 4. Postoperative picture 4 months after surgery.
CLINICAL CASE Nº 3.
| FRAGMENTATION MISSILE IN THE LOWER EXTREMITY |





CLINICAL CASE Nº 4.
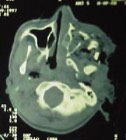
HIGH VELOCITY GUNSHOT WOUND IN THE FACE






Sus datos no son tomados sin su permiso.